Category Archives: Congenital Heart Disease
Service or Martyrdom?
This is a retro-blog.
I remember one patient who was referred to me for neonatal care. It was about 4 years ago. A mother had to deliver prematurely by cesarean section because of premature rupture of membrane and uncontrolled uterine contractions.. Baby was 28 weeks gestational age. There was no more room for control of labor, and preparing the baby’s lungs for eventual delivery; the cesarean section had to be done outright. Both parents were employed at that time, so I thought there was no problem about financial resources.
Again, as for all babies being born prematurely, he needed to be administered surfactant. It was night time, banks were closed so there’s no way the father can tender cash at that time. I told him to go to another hospital, secure surfactant with my name as guarantor and sign a waiver for them to pay for the drug in 24 hours. The medicine was released to him and thus I was able to administer it immediately.
(Image courtesy of www.nhlbi.nih.gov/health/health-topics/topics/pda/)
Baby was already being weaned from the respirator, when a new problem arose, a patent ductus arteriosus. This posed a threat as it increased the volume of blood that goes to the lungs for oxygenation and predisposing to a chronic problem: bronchopulmonary dysplasia. Oral medication given via tube to treat the problem. Then another problem set in: persistent pulmonary hypertension and renal insufficiency bordering renal failure, plus signs of systemic infection showing. I did some double volume blood exchange transfusion here besides giving respective medicines.
Baby’s persistent pulmonary hypertension responded to sildenafil. After the exchange transfusion, baby started urinating. Then the murmur disappeared. However, it took a some time to wean the baby off from the respirator because of one problem: baby developed bronchopulmonary dysplasia. I had to give cocktail of medications. Finally baby was weaned off from the respirator and was extubated but still dependent on oxygen support. There were even times when after extubation and when his BPD would exacerbate, it would require some hourly aerosolization to open up his distal airways.
When baby was almost two months, he was then discharged from the hospital, free from oxygen support, feeding well, and gaining weight daily. Due to big hospital bill, they asked if it is okay for them to sign a promisory note for their payment of my professional fee. Should I say no? I never proposed any condition at all. I just called the hospital to give my approval. They also partially paid their hospital bill.
One week from discharge, they followed up at the clinic. Few days after that, the hospital declared bankruptcy and closed. Then, my fear came true. They disappeared and never came back. They never at least had the courtesy to tell me that they can’t pay my professional fee. Nada! Boom! Ba-bye! I had their number. Sometimes I ask my secretary to remind them, but then they just say they will come to no avail. Then I recall how was I attending to that baby before, I had no car then. I would wait for a cab to visit the baby. Then during early mornings, I had to walk for about 10-15 minutes going to the main road to hail a cab to go back home. And then this is what I deserve.
The perks of a neonatologist. Other colleagues surely do have their own stories and could be worse than this.
My Blue Baby
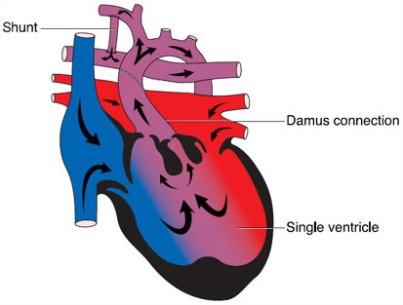
(Image credit: http://www.lhm.org.uk/info/surgical-treatments-for-right-sided-single-ventricle-conditions-48.aspx)
On that day that I admitted three babies successively, there were two premature babies who immediately presented with respiratory distress (of course, it’s expected & understandable), and a full term. I thought that the full term baby was unremarkable until a few minutes after birth when he himself presented with respiratory distress. Initially, I thought it was because of fluid retention in his lungs that caused him to be breathing fast and appearing “bluish.” Fluid retention is usually a common disorder usually experienced by babies delivered via cesarean section (whose mothers did not undergo labor). To some extent, vaginally born babies may also experience transient tachypnea due for fluid retention especially if the labor was precipitous (shorted period than expected). Fluid retention usually resolves in six hours in most babies, but in few cases, may last up to 2-3 days. Babies presenting with such condition will not usually require antibiotic treatment, and will respond often to mere oxygen administration. I initially started the baby on oxygen inhalation.
On the sixth hour of life, the baby remained with fast respiratory rate (tachypnea). We did an x-ray and did a blood test for a marker of infection. Chest x-ray was suggestive of pneumonia whereas the infection marker was non-reactive. Initially, I did not agree with the x-ray findings because the baby has no risk factor of having an infection so I did not start antibiotics yet. The baby’s respiratory rate actually normalized few hours afterwards, but his oxygen saturation was always low, especially when active and crying. This patient’s status and presentation is not compatible with the classical pneumonia cases. Nevertheless I was forced to start antibiotics (at the back of my mind, it’s better act than be sorry if in the end the baby has also a concomitant infection). On the third day, baby remained comfortable, with normal respiratory rate, however, still bluish especially when the nasal cannula delivering the oxygen gets accidentally dislodged from his nostrils. We also noted that the heart beat was stronger in the right side than in the left (which is the normal location of the heart’s tip or apex, and thus stronger heart beat is supposedly appreciated louder from that side). I was considering now that this might be a heart problem. I requested for a repeat chest x-ray to confirm my suspicion of a dextrocardia. (Dextrocardia means that the heart apex is located in the right side, contrary to the normal).
(Image credit: http://estudandoraras.blogspot.com/2009/05/dextrocardia.html)
Few hours earlier, the baby was evaluated by a cardiologist. A 2D Echocardiography was done and revealed a dreadful finding, it sealed the baby’s fate. The baby indeed has a dextrocardia, but on top of that are more serious findings: situs ambiguous, single atrium, single ventricle, large patent ductus arteriosus, and moderate pulmonary hypertension. This just means, his heart is like that of a fish. I was literally dumbfounded when the cardiologist told me his findings. I dont know how the mother can take it when I will talk to her but I am glad that the burden of telling the mother went to the cardiologist. He would be in a better position than I explaining the baby’s condtion. This would be too heartbreaking on the side of the mother, especially so that she plans to leave for the Middle East after one month to work. Question now is, will she wait for the baby to die before she leaves?
— UPDATE—
Few days after, yesterday to be exact, mother sent me an SMS that baby finally expired. May God bless his soul and take him to His kingdom.