Are You Aware? New Global Causes of Child Mortality & Breastfeeding.
Category Archives: Breastfeeding
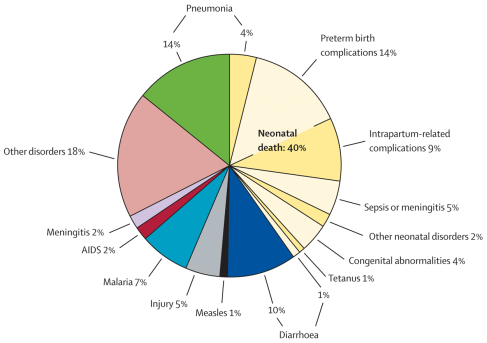
New Global Causes of Child Mortality Data Released in Lancet, May 2012. (Reference: Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. (2012) The Lancet, Early Online Publication, 11 May 2012 doi:10.1016/S0140-6736(12)60560-1)
- The burden of mortality in children younger than 5 years varied widely across WHO regions in 2010, with the largest number of deaths seen in Africa (3·6 million) and southeast Asia (2·1 million). Breastfeeding has and is playing a crucial role in the survival of the infants.
- In 2010, neonatal mortality was highest in southeast Asia (1·096 million deaths, 52·3% of regional deaths in children younger than 5 years), with 19·2% of deaths (0·402 million, UR 0·262—0·558 million) attributable to preterm birth complications, and 21·8% of deaths (0·457 million, UR 0·359—0·551 million) attributable to pneumonia in the neonatal and postneonatal periods.Of the WHO
NEONATAL MORTALITY – HIGHEST CONTRIBUTOR TO CHILD MORTALITY
The majority of mortality is being contributed by the newly born population. Perinatal mortality has been defined as mortality of either of the mother-infant dyad during the perinatal period, which is defined as the period from 20th week of gestation to seven days after birth. Infants dying in their first week of life then highly speaks of the quality of prenatal care their mothers received. On the other hand, infant deaths occurring between seventh to the 30th day reflects the quality of infant care and may not necessarily a sequela of prenatal care.
A good question to ask is, when do these neonates die? In a data review of the deaths of neonates by day locally, it showed that most infants do not survive more than 48 hours, with a declining incidence towards the end of neonatal period. This first 48 hours of life still coincides with the perinatal period, which then clearly underscores the fact that majority of our mothers are not receiving optimum and adequate prenatal care thus leading to their demise.
Deaths of Neonates by Days, Philippines 1998-2003. (MA Silvestre, 2009).
There has been increasing preterm birth in the last few years, and preterm birth complications have contributed significantly to mortality burden among children before their fifth birthday. Locally, pregnancies are terminated prematurely because of urogenital infection (triggering preterm labor), uncontrolled maternal hypertensive disorders, abnormal bleeding (placenta previa, abruptio placenta). Having adequate access to mother-child care providers will significantly improve this saddening statistics. The PhilHealth recently reported that out of the 1400 plus cities and municipalities, only 607 cities and municipalities have mother-child care facilities; LESS than 50%.
PNEUMONIA, SECOND HIGHEST CONTRIBUTOR TO CHILD’S MORTALITY.
The peak incidence of mortality from pneumonia is the first six months of life. Pneumonia is a vaccine-preventable disease. There are currently two conjugated and one polysaccharide pneumococcal vaccines available in the market. Of these, it’s the conjugated vaccines that can protect the infant from pneumococcal death during the first six months of life, as the polysaccharide vaccine can only be administered when the child is at least 2 years of age. Unfortunately, the conjugated pneumococcal vaccine is not available in health centers due to its high cost. Majority of the population that flock to the government vaccination centers, who cannot avail of the said vaccine, are therefore vulnerable to succumb to this disease.
The newly born infant’s immune system is inexperienced, thus any infection immediately at birth may lead to infant’s death. During pregnancy, whatever antibodies the mother has through vaccination or active infection are shared to the fetus through the placenta. (Problem lies when the mother never had infection nor vaccination, there would be nil to share). These antibodies may be the only armamentarium the infant has, however do not confer absolute protection after birth, and wanes by around six months of life. However, mother also continues to provide additional antibodies to the baby after birth during breastfeeding; a process cow milk formula can and will never duplicate.
A person has two manners of acquiring antibodies – active: by producing during vaccination or active infection; and passive: through infusion of already formed antibodies during pregnancy, breastfeeding and infusion of immunoglobulin concentrate. Vaccination is a process whereby a weakened antigen (whether the organism itself of its by-product) is introduced to the individual in an attempt to trigger his immune system to produce antibodies against the offending organism, but the antigen is not strong enough to cause infection or disease by itself. Pneumococcal vaccination should then be accomplished during the infant’s first six months of life to preclude this peak incidence of death from pneumonia during this period.
What has been noticeable though, according to the article, was the mention of how breastfeeding is playing a crucial role in the survival of these infants.
WHEN TO INITIATE BREASTFEEDING?
Delaying the initiation of breastfeeding is HARMFUL!!! In an observational cohort done at Ghana, observing 10,492 infants who survived beyond their 48th hour from birth, the following were the findings:
- there is an increased risk of death from infection with increasing delay of initiating breastfeeding;
- if the breastfeeding was initiated only after 24 hours of life, there is a 2.6-fold risk of death;
- moreover, if initiation was delayed, the infant was partially breastfed (meaning baby was also given cow milk formula), the risk increases to 5.7-fold. (Reference: Edmond KM, et al. Effect of early infant feeding practices on infection-specific neonatal mortality: In rural Ghana. Am J Clin Nutr. 2007; 86:1126-31.)
In Southern Nepal, frequent home visits were done among 22,838 breastfed newborns, who survived beyond 48 hours. It was noted that
- in the first hour of life from birth, only 3.4% were breastfed;
- within 24 hours of life, 56.6% of infants were breastfed;
- babies who were partially breastfed (72.6%) were at higher mortality risk than exclusively (purely) breastfed infants- the longer the delay of initiating breastfeeding, the higher mortality rate;
- mortality was higher among late (>24 hours) than early (<24 hours) initiators
- neonatal death may be avoided if breastfeeding is initiated within first day or 24 hours of life (7.7%), but more when initiated within the first hour of life (19.1%). (Reference: Mullany LC, et al. Breast-Feeding patterns, time to initiation, and mortality risk among newborns in Southern Nepal. J Nutr, 2008; 138(3):599-603).
WHAT PHILIPPINES HAS DONE AND IS STILL DOING….
- provision of warmth and drying of the infant, simultaneously stimulating him to breath;
- uninterrupted skin-to-skin contact — this procedure allows baby to acquire maternal bacterial flora that will colonize his intestines that will serve to prime his immune system, delays onset of allergic disorder, and positive effect on the duration of breastfeeding (likelihood of prolonged breastfeeding);
- delayed cord clamping – helps prevent iron-deficiency anemia; and
- initiation of breastfeeding within the first 90 minutes of life.
(Unang Yakap video may be viewed in this link: http://www.youtube.com/watch?v=5hCP7rYHrwA)
The DOH with Bureau of Food and Drugs has also strictly implemented the Milk Code. Among the provisions of milk code are:
- exclusive breastfeeding for 0-6 months;
- no substitute nor replacement for breastmilk;
- appropriate and safe complementary feeding should start from six months onwards in addition to breastfeeding;
- breastfeeding is still appropriate for young children up to two years of age and beyond;
- infant or milk formula may be hazardous to a child’s health and damage child’s formative development;
- advertising, promotions or sponsorships of infant formula, breastmilk substitutes and other related products are prohibited;
- other related product such as, but not exclusive of, teats, feeding bottles and other feeding paraphernalia are prohibited in health facilities;
- government and all concerned stakeholders must continuously accomplish an information, dissemination campaign/strategy, and do further research on the advantages of breastmilk and the hazards of breastmilk substitutes or replacements; and
- milk companies, and their representatives, should not form part of any policy-making body or entity in relation to the advancement of breastfeeding.
Are You Aware? New Global Causes of Child Mortality & Breastfeeding
Breastfeeding Dilemma: Flat Nipple Correction
Breastfeeding is one avenue where woman achieves fulfillment and contentment as a woman, a successful mother, that is. The act entails the mother to offer her bossom not only to nourish but sustain that life that emanated from her womb, become fit and healthy individual. While some woman achieves this gratification, some woman however fail and deem unfit as a mother. Women with flat or inverted nipples for instance fail inadequate as a mother and could affect them psychologically.

Fortunately, there’s a remedy to address this problem. Several online sites may be referred to on these subject matter but I’d like to share a local management that with do during delivery and while establishing breastfeeding.
All you need is pair of scissors and a 10mL syringe.

1. With your pair of scissors, cut the end where the needle is attached to make it appear like this.

2. Remove the plunger, then insert through the cut end so that the tip of the plunger will now approximate the blunt end, as shown below.

3. Then appose the blunt end to the nipple. Pull the plunger creating a vacuum effect that will “pull” the nipple up.

Do this repeatedly until the desired result is achieved, i.e., the nipple would be easily grasped by the baby.

(before)

(after)
Thank you for reading and sharing.
this method/technique is not my own; I am not aware though who originally thought of this technique. I acquired this from my senior residents and employed it during my training, and until now.)