I got an interesting referral from one hospital. It is not really that difficult of a case but it is quite puzzling for the untrained ones, nevertheless interesting.
The mothers’s history is generally unremarkable. She only had some flu-like symptoms during the last trimester of the pregnancy. There was no history of hypertension nor diabetes. Mother’s prenatal visits were timely and regular as this is very much wanted pregnancy. Generally, she never had symptoms. She came to the hospital in labor. She had an ultrasound which stated that the baby is in fine condition, there was adequate fluid. About 12 hours into delivery the bag of waters ruptured. The mom recalled that she noted the fluid to be yellow-stained (normally it should be clear). There was no foul odor.
She gave birth by normal vaginal delivery. The baby was not that big, weighing only 2.6 kgs. There was no difficulty during baby’s delivery. There was no cord loop around the neck (that may have strangulated the baby). The fluid was viscid, thickly saturated with meconium (baby’s first stool). Few minutes thereafter, the baby began to have respiratory distress requiring oxygen support.
Baby had an xray of the chest revealing pneumonia. He was then started on empiric broad spectrum antibiotics. Baby was nursing well from the mother while on oxygen supplementation. There was no progression of the respiratory distress. Despite requirement for oxygen, baby remained comfortable. On the 5th day of life, baby still cant be weaned off from oxygen, breathing was still fast although comfortable. Repeat xray of the chest revealed significant clearing of the pulmonary infiltrates initially seen on the previous xray. An arterial blood gas analysis was done but it was unremarkable. So why then is the baby requiring oxygen despite the comfortable breathing, normal blood gas analysis and clearing of xray picture?
The baby was then referred to me at this time. At first I went with the line of unresolved infection so I suggested shifting of antibiotics as well as determination of c-reactive protein (an indicator of inflammation – often due to infection, that may as well be used to monitor response to treatment).
The CRP was reactive, meaning it indicated presence of an ongoing inflammation/infection, but the value was not congruent with the distress of the baby. So I tried to play along with some of the facts that the baby presented. First, baby was born throught thickly meconium stained amniotic fluid. Second, the baby’s initial xray findings highly suggested pneumonia. Third, the baby remained oxygen dependent despite ample time for antibiotics to have worked, granting this was supposed to be an isolated pneumonia. Fourth, despite improvement of x-ray picture, the baby remained, clinically, unimproved; was still dependent on oxygen support.
With these, I came to rationalize that baby might be having meconium aspiration pneumonia (MAP). (While meconium is supposed to be sterile , meaning it is free of bacteria, antibiotics was a rational modality of treatment as CRP was reactive). But on top of the MAP, I considered that baby might be experiencing as well a complication.
I then requested to obtain blood gas analysis from the right and the left arms, with emphasis on the pulmonary oxygen between the two sites.
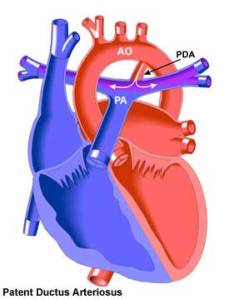
The aorta, the main vessel that arises from the left ventricle (red vessel creating a loop on the above illustration) gives rise to three large vessels that supply the upper part of the human body. The first branch immediately divides into two, one serving as right subclavian artery (that which supplies our right arm) and right carotid artery (that branch supplying to the blood). The second main branch becomes the left carotid artery which also supply our head on the left side whereas the third main branch is the left subclavian artery which supplies our left arm.
There usually is a ductus arteriosus that exists in the fetus and closes permanently about 10 days after the baby is born. It usually arises after the right subclavian and carotid arteries, and before the left subclavian artery. Thus, by origin, the right subclavian artery is usually termed preductal while the left subclavian artery may be, most often, post-ductal. Since preductal vessels include those vessels that send blood supply to the brain, it is also then safe to assume that preductal blood picture also reflects the same blood picture that goes to the brain.
In cases of pathology when the pressure in the right side of the heart is higher than that of the left, and the ductus artery is still patent/open, the unoxygenated blood in the right side may dilute the already oxygenated blood in the left through the ductus arteriosus. In cases therefore involving increased right-sided pressure, the baby tends to be cyanotic from this explanation.
One way of determining whether there is a significant shunting from the right side to the left side via the patent ductus arteriosus is performing a 2-D echocardiography, which exactly measures the pressures between the two sides of the heart. Just compare your obtained pressure from the right side of the heart with the normal values for age and you can immediately say there is elevation of pressure, or simply put pulmonary hypertension. Another way of determination is to obtain blood gas from preductal (right arm) and post ductal (left arm, right foot, left foot) extremities. Then, compare the partial oxygen tension/pressure (pO2). A gradient between right and left of more than 20 mmHg is highly suggestive of right sided pressure, in this case, persistent pulmonary hypertension, of the newborn (also known as persistent fetal circulation).
The baby’s right arm blood pO2 was 81.7mmHg, whereas the left arm pO2 was 42.16mmHg. There was a gradient between right and left arm of 39.1mmHg, way higher than 20mmHg cut off, clearly suggesting that the baby has a pulmonary hypertension. Pulmonary hypertension usually arises when the small supposedly thin capillaries in the lungs that carry blood for oxygenation thickens. With thick pulmonary vessels, the transit of oxygen from lung alveoli to the blood vessels is rendered more difficult and hence the slow or lack of oxygenation of the blood that returns to the heart, making the baby a little bluish. And if the pulmonary hypertension is severe, this “resists” the incoming blood from the heart and is shunted directly into the aorta via the ductus arteriosus, unoxygenated, already diluting the blood that may have successfully went into the lungs for oxygenation (but not sufficiently). This can turn into vicious cycle until the baby’s demise.
(photo courtesy of http://trialx.com/curebyte/2011/07/13/clinical-trials-and-related-photos-for-persistent-pulmonary-hypertension-newborn/
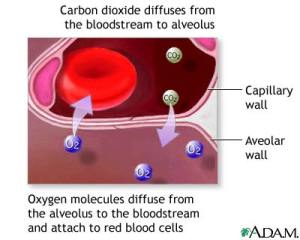
(photo courtesy of http://www.pennmedicine.org/health_info/body_guide/reftext/html/resp_sys_fin.html)
In cases however of pulmonary hypertension, where the wall between the right and left atrium has a large communication known as patent foramen ovale, since at the level of atrium there is already mixing of blood between right (unoxygenated) and left (oxgenated) sides of the heart, there may not be an appreciable gradient of pO2 between preductal and postductal blood gas analyses.