UN resident representative described the Philippines as the “worst performer” in Asia as far as achievement of Millenium Development Goals (MDG) are concerned. This, as far as lowering of child mortality, decreasing maternal morbidity and mortality as well as HIV prevention are concerned.
These three are included in the Responsible Parenthood and Reproductive Law that was already signed, implementing rules and regulations signed as well, but put on hold by the “status quo ante order” issued by the Supreme Court on March 19, 2013.
This law went through hurdles for about 16 years before being finally passed by the 15th Congress. It aims to empower people by making them a responsible parent. By this, it will allow parents to determine the number of their offspring they can responsibly have – those that they can feed, vaccinate, send to school and be a responsible citizens of the country. This can be achieved through sexuality education, which will be taught while the children are young, and employment of safe and acceptable contraceptive methods, depending on the couple’s choice, heightened HIV education and awareness especially to population at risk.
Recently, there was a scandal about an adolescent college student who claimed her life after, bottom line, cannot afford to pay her tuition. They are 4 siblings and yet the father cannot afford her tuition fee. And how does this relate to the RH Law? I am not saying the father is irresponsible. BUT, had he considered that he could only afford to rear one or two children, providing all their needs, then his daughter wouldn’t have suffered this problem at such a young and tender age. He could still have his brilliant daughter this very minute with him.
I am the eldest of 4 children. My parents used pills and condoms. We don’t own a house and we had been renting up to this date. When I was about to enter the school of medicine, the 4 of us were already simultaneously going to college. With my father’s income, he couldn’t afford to send us altogether. He talked to me that he cannot afford my tuition. If he would, my other siblings wont be able to enrol. I on the other hand has graduated from college already, so perhaps I could already work and save up for my tuition. I was heartbroken as my aspiration of being a physician was imperiled. I won’t be graduating with my batch mates. I felt it was so unfair for me. I was selfish as I didn’t want to trash my dreams to happen at the right time that I want it to, and without considering my other siblings’ welfare too. But my selfishness was my motivation and determination to find myself a scholarship that can fuel my ambition. My youngest sister as well was able to secure a scholarship for her. So basically, my father was only supporting two of my other siblings as far as tuition and miscellaneous fees are concerned. It was very very difficult time. Sometimes we have to make do with our meager allowance. But one thing I salute my parents for was that we were never delayed in paying our tuition. My parents didn’t want as much as possible for us to be delayed from graduating. They didn’t want as much as possible for us to be working scholars in order for us to afford college. As much as possible, they wanted to shoulder the entire burden of sending us to college as it is their obligation to do so. They believed it was was their duty and responsibility. My parents admitted that they won’t be able to give us land, house or any property for inheritance but our education that will help us build our own future. Now, if my parents who practiced family planning were still hard up to give us good and quality education, how much more for those who had not?
I am aware of that it will be a long time before the concrete effects of RH Law will be experienced by our fellowmen. But delaying it or even preventing it from being implemented, considering our country’s situation right now, is a violation of our rights to access to reproductive health care. We need an immediate tangible effect such as in the following case.
Small for Gestational Infant
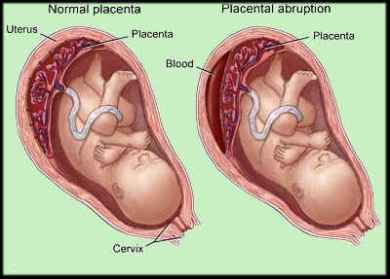
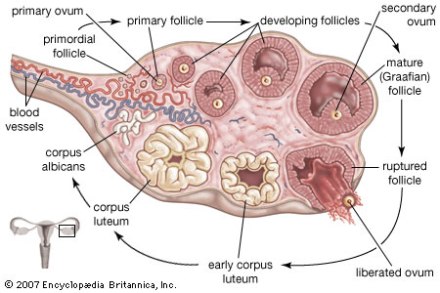
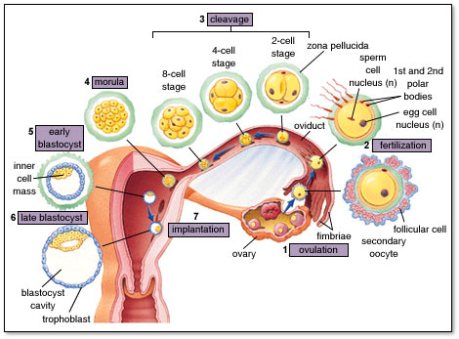
A mother conceived, she was hypertensive even at the early stages of her pregnancy. After reaching 20 weeks, her blood pressure all the more shoot up. Even with medical care from a private obstetrician, still the blood pressure wasn’t adequately controlled. At 36 weeks, she came to the hospital in active labor. The baby’s heart beat was erratic and had to be delivered immediately, or else we will lose the baby.
The baby came out without spontaneous breath and crying, and the heart beat was very slow. He had to be resuscitated, a tube was inserted into his trachea to assist him breathing. He was small for his age of 36 weeks, with respect to his weight, length and head circumference (an indirect indicator of brain growth). This only means that the baby was chronically “undernourished” inside the mother’s uterus that’s why all of his anthropometric measurements were below normal.
Adequate blood glucose and oxygen supply from the placenta to the baby is necessary for optimum brain and body growth. Normal or good glucose level stimulates the production of more insulin-like growth factor 2, which is responsible for increasing the number of neurons and oligodendrocytes, and increasing the communications between neurons through dendrites and axon. An increased communication between these two parts of neurons leads to faster transmission of signals. Bottom line, intelligent kid. The opposite, “bobo.” I am not saying this is always the case but the risk, a very high risk at that, to being one is undeniably there.
So this baby already suffered an injury biochemically and physiologically inside the womb, even if he was born alive. So it’s true no mother died in this case. It’s true, no baby died in this case. But the impact of the chronic uncontrolled hypertension to the baby’s brain, IS permanent, and may be debilitating. This thing is still happening among our pregnant mothers, even if they are under the care of able obstetricians. But what about those who have no access to obstetricians? And mind you, this is just one aspect of issues surrounding a pregnant woman. There are more other pressing equally important concerns.
One anti-RH bill argues that there is no more need for RH law as there is already an existing Magna Carta Law for Women. Let me throw back the question to you. With the MCW in place, how come, we still have this high incidence of maternal morbidity and death? With the MCW in place, how come we are not achieving the millenium development goals? And what about HIV which is not included in the MCW, neonates? With the SQAO against implementation of the RH Law, aren’t we not endangering further our poor constituents? Is it right to issue this SQAO at this time?